Given the advances in 3D printing technology in the last year, it’s no surprise that in the season finale of the TV show Grey’s Anatomy, Dr. Cristina Yang leaves Seattle to continue her cardiac surgery research at a fictitious state-of-the-art facility in Zurich — a facility equipped with dozens of 3D printers.
In the real world, 3D printing technology is opening up a wide variety of possibilities for medical advances. Bioengineers are using 3D printers to manufacture all kinds of replacement body parts, such as tracheas that gave breath to Baby Kaiba (2013) and Garrett Peterson (2014), ears and noses, jawbones, kidneys and other internal organs.
In the basement of the Children’s Hospital at the University of Colorado’s Anschutz Medical Campus, Dr. Richard Weir and his research assistant Stephen Huddle are using a 3D metal printer, one of only a few currently in use in the United States, to bioengineer robotic fingers and hands. I was lucky to see this leading edge innovation and hear from the scientists in person as part of the field trip day at Health Journalism 2014, the annual conference for the Association of Health Care Journalists held in Denver in March.

My hand, holding a 3D-printed metal finger. Metal-printed prostheses are stronger than plastic, a significant benefit for body parts like hands and fingers, which people are more apt to use roughly in daily life.
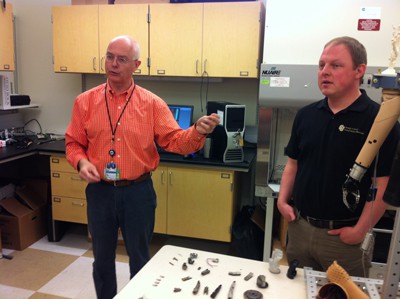
Dr. Richard Weir and research assistant Stephen Huddle explain their bioengineering design and research.

3D metal printer in progress, making a prosthetic palm
After providing an overview of the technology, the scientists showed us the 3D metal printer in action, making a palm all-in-one-go. The printer looked like a giant microwave oven. The triangular arm you see inside the printer window on the left swept across and sprayed a thin layer of metal powder, 20 microns thick. (A micron is a millionth of a metre.) Next, laser light from above welded the powder in place to the palm being printed on the work surface. When the welding was completed in a matter of seconds, the work surface moved down 20 microns to make room for the next sweep of metal powder. This process is repeated over 14 hours to 2 days to produce a finished piece.
It was very cool to see the printer in operation, but we learned that 3D printing is only one part of the innovation to make robotic hands and fingers. For the last decade, Weir has been collaborating with the Alfred Mann Foundation, the Illinois Institute of Technology and Sigenics, Inc. to develop implantable myoelectric sensors (IMES), sensors that can be implanted under the skin to read muscle signals.

IMES: implantable myoelectric sensor
The goal is to create a hand that can move with the same full range of motion as a human hand, a big leap forward from existing prostheses that can only open and close in sequence. “If we can go into each of the 18 muscles in the forearm with sensors that give 18 control signals rather than what we have at the moment, that would advance the science,” said Dr. Weir. Together, 3D metal printed artificial arms and implanted sensors promise to offer plug and play functionality for people who have lost limbs.
Right now, the IMES technology is being tested by Staff Sergeant James Sides, a veteran who lost his forearm in a blast injury. He has 8 IMES sensors implanted in his forearm. In this video, he explains how the technology allows him to move his hand with simultaneous motion and lets him separately move his thumb, a big improvement over existing “dummy” prostheses.

