In the last several years, there has been a flood of health news about studies linking vitamin D deficiency with cancer, cardiovascular diseases, diabetes, metabolic disorders, depression, infectious diseases, autoimmune diseases, mortality and even autism. A search on PubMed for vitamin D finds more than 1,400 papers listed from January to April 2014 alone.
As a result of this increased interest, some people are boosting their intake above the recommended dietary allowance hoping that extra vitamin D might help prevent, treat or cure a host of adverse disease conditions.
Vitamin D supplementation is proven to be effective to help maintain good bone health, but can increasing intake above the current recommended dietary allowance really cure or prevent other health conditions?
Vitamin D and arthritis
Dawn Hunter, a freelance editor based in Toronto, Ontario, takes 2,000 IU (international units) of vitamin D daily, even though some health guidelines call for a much smaller dose of 600 IU per day. “Every time I stop taking it, my levels just plummet,” says Hunter, who has arthritis and says that she does not have the opportunity to get much natural sunshine.
Five years ago, Hunter found out she was severely deficient after her rheumatologist ordered a blood test. She addressed her deficiency by taking 4,000 IU daily for a year to boost her blood level from 14.8 ng/mL (nanograms per milliliter) and has been maintaining her level at 30.4 ng/mL with a daily dose of 2,000 IU for the past 4 years. (The normal range is 30.0 to 74.0 ng/mL).
“When my vitamin D level increased, I noticed a small reduction in the general ache I had with my arthritis,” notes Hunter. “My rheumatologist says there is some evidence that arthritis can progress faster in people who have low levels of vitamin D. I was just turning 40 when my arthritis was diagnosed, so managing progression is important to me.”
Vitamin D is really a hormone
Vitamin D is actually a pro-hormone that is involved in many metabolic processes. Your body makes vitamin D from sunlight on your skin. You can also take supplements and you can get a small amount from fortified food sources such as milk or orange juice.
Supplements come in two formats: vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol). Vitamin D2 is found naturally in sun-exposed mushrooms. Vitamin D3 is the form made naturally in human skin and is made from a cholesterol precursor obtained from lanolin. It can be found in oil-rich fish like salmon, mackerel and herring. There is some evidence that the D3 format is more bioavailable. Vitamin D is fat-soluble, meaning that if you take too much, the excess is not excreted in urine.
In your body, your liver converts vitamin D from sunlight or supplements to 25-hydroxyvitamin D, [25(OH)D], the form that is measured in a blood test. The 25 (OH)D is then converted again, mostly in the kidneys, to the activated form of vitamin D, a hormone called calcitriol (1,25-dihydroxyvitamin D).
It’s plausible that vitamin D may play a role in a host of other diseases and conditions such as cancer, cardiovascular disease and diabetes because there are calcitriol receptors on nearly all tissues in the body. Calcitriol plays a role in the regulation of over 900 different genes. In cell culture and animal studies, researchers have found that calcitriol is involved in cell differentiation, proliferation and inhibition, inflammation, and the synthesis and secretion of insulin. Calcitriol also has an impact on brain function and development. Two U.S. researchers recently proposed a mechanism to explain how calcitriol may be involved in the regulation of the production of serotonin, a brain chemical that is often out of balance in autistic children.
At first blush, it may seem hard to believe that vitamin D could be associated with so many different conditions. However, John J. Cannell, MD, Founder and Executive Director of the Vitamin D Council, says, “Many people are turned off by these claims and say it’s impossible that one thing is involved in so many different disease processes, but they are unaware of the mechanism of vitamin D. It is actually a steroid hormone precursor that turns genes on and off. There are at least a thousand genes that are directly regulated by vitamin D.”
Recent vitamin D studies
Here are some examples of recent studies that found a link between vitamin D and health conditions.
Cholesterol
Vitamin D may improve cholesterol numbers. A recent study analyzed data from 576 postmenopausal women who were part of the National Institute of Health’s Women’s Health Initiative trial. Women who took 400 IU of vitamin D plus 1,000 mg of calcium daily showed a significantly higher blood level of vitamin D after two years, compared to the control group who took a placebo. Interestingly, those who had higher blood levels of vitamin D also had better lipid profiles, showing increased high-density (“good”) cholesterol), decreased low-density (“bad”) cholesterol and lower triglycerides. The researchers acknowledge that the sample size was small and their findings are not conclusive about how vitamin D affects cardiovascular health. However, given that these results were from blood work for women followed for several years, there is a relationship here that merits further research. The study was published in the March 2014 issue of Menopause.
Breast cancer
Patients with higher levels of vitamin D at the time of breast cancer diagnosis may live longer. A recent meta-analysis combined data from more than 4,500 breast cancer patients from 5 observational studies to see if higher vitamin D levels at the time of breast cancer diagnosis were associated with longer patient survival times. Over a 9-year period, patients in the group with the highest blood level of 25-dihydroxyvitamin D [25(OH)D], (the form of vitamin D measured in blood tests), at an average level of 30 ng/mL, had about half the fatality rate compared to those in the group with the lowest level of 17 ng/mL on average. In the paper, researchers reported that other lab studies have shown that vitamin D has anticancer effects, arresting tumor growth in 3 critical phases of development. While these results are encouraging, the researchers caution that a causal conclusion is not possible and that a randomized controlled trial is needed to shed further light on the findings. The study was published in the March 2014 issue of Anticancer Research.
Risk of Mortality
Low vitamin D levels carry a greater risk of death. In a large systematic review and meta-analysis published in the April 2014 issue of the British Medical Journal, researchers looked at the link between vitamin D and chronic diseases to assess mortality risk. They combined data from several large databases of studies, including Medline, Embase and the Cochrane Library. Low blood levels of vitamin D were associated with a greater risk of death from cardiovascular disease, cancer and other causes. Calculations showed that each 10 ng/mL decline of 25(OH)D was associated with a 16% greater risk of mortality and that supplementation with vitamin D3 reduced mortality risk by 11%.
Autism
Vitamin D may play a role in abnormal social behavior seen in people with autism spectrum disorder. Rhonda Patrick, PhD, and Bruce Ames, PhD, at the Children’s Hospital Oakland Research Center (CHORI) in California, proposed a causal mechanism for how 3 brain hormones that influence social behavior — serotonin, oxytocin and vasopressin — are activated by vitamin D at the genetic level. These brain hormones are often out of balance in children with autism spectrum disorder. These researchers hypothesize that the drop in adequate levels of vitamin D in the U.S. over the past few decades — due in part to increased use of sunscreens and more indoor work — may in part explain the increase in autism rates. The study was published in the February issue of The Journal of the Federation of American Societies for Experimental Biology.
Different views on the ideal level of vitamin D?
Almost 70% of the U.S. population has insufficient levels of 25(OH)D, when defined as less than 30 ng/mL, according to data combined from many studies. The level of vitamin D in your body is measured by a blood test that measures 25-hydroxyvitamin D, [25(OH)D], the form of vitamin D that your body makes after converting what you receive from sunlight on skin, supplements or from some food sources, such as fortified milk and orange juice or from the flesh of fatty fish, including salmon, tuna and mackerel. The Vitamin D Council, a nonprofit organization based in California that works to educate the public about vitamin D, notes that there are several factors that affect how much vitamin D your body produces when your skin is exposed to sunlight. These factors include the time of year and time of day of exposure, where you live and the type of skin you have. You can request a blood test to check your vitamin D levels from your doctor, and the cost is usually covered in the U.S. if a doctor orders it with the right diagnostic code.
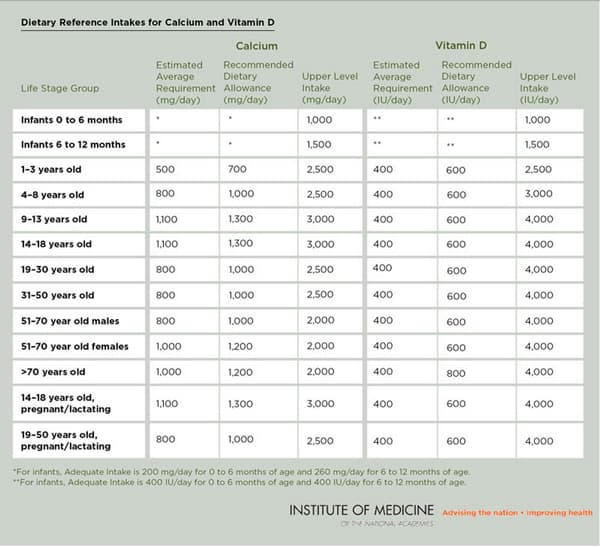
According to the Institute of Medicine (IOM), the current recommended dietary intake of 600 IU for adults under the age of 70 years and 800 IU for adults over 70 years is sufficient to meet the needs of 97.5% of healthy adults who have minimal sun exposure. The IOM defines sufficiency of 25(OH)D as greater than 20 ng/mL. This recommendation was based on proven benefits for bone health, as the IOM did not find convincing evidence about causal outcomes with other health conditions.
The Vitamin D Council recommends a much higher daily intake of 5,000 IU to achieve a sufficiency level of 50 ng/mL. Dr. Cannell says, “The Vitamin D Council arrived at a recommendation very simply — to reproduce natural vitamin D from sun exposure. We know that natural vitamin D levels for lifeguards and roofers and hunter/gatherers from modern-day Tanzania are about 50 ng/mL. Until all the studies are done and all the science is completed, the safest thing for you to do is to maintain a natural vitamin D level.”
The IOM, however, noted a concern for attaining levels above 50 ng/mL and designated 4,000 IU daily as the tolerable upper intake limit, with the caution that this is not to be interpreted as a target intake level. JoAnn E. Manson, MD, DrPH, Chief of Preventive Medicine at Brigham and Women’s Hospital and Professor of Medicine at Harvard Medical School, was on the IOM Committee that developed the guidelines. She says, “There’s still a pretty wide range of intake in the IOM guidelines. The recommended dietary allowance is what will meet the requirements for a very large majority of the population, 97.5% in the U.S. and Canada, but the IOM is also saying that there is a risk of adverse events at intake levels above 4,000 IU per day.”
Risks of too much vitamin D
How much is too much? Observational studies suggest that shooting for blood levels above 50 ng/mL may be associated with an increased risk of pancreatic cancer, cardiovascular disease and an increased risk of death. Dr. Manson says, “Some vitamin D is good, but more is not necessarily better. People should understand that there is limited research on long-term intakes above 2,000 IU daily. If they are regularly taking 3,000-4,000 IU per day, even if those levels may not have been linked to adverse events, we do not know if the benefits outweigh the risks long-term because we don’t have the evidence.”
Massive doses of 10,000 IU daily or more can put you at risk of developing high calcium levels in the blood, or in the urine, which could cause calcification of blood vessels, kidney problems and kidney stones, especially if calcium intake is also high.
Dr. Manson advises that it’s important to distinguish between public health guidelines and medical situations where individual patients actually need more vitamin D, such as those who have bone health problems, malabsorption or who are on medications that may interfere with the metabolism of vitamin D. For example, steroid drugs like prednisone, weight loss drugs like orlistat (Alli) and the cholesterol-lowering drug cholestyramine (Questran) can reduce the absorption of vitamin D.
The National Institute of Health (NIH) identifies a number of interactions of moderate concern, including with the cholesterol-lowering statin Lipitor: “Atorvastatin (Lipitor): Vitamin D might decrease the amount of atorvastatin (Lipitor) that enters the body. This might decrease how well atorvastatin (Lipitor) works.”
While there may be some situations that warrant higher doses of vitamin D, Dr. Manson cautions against taking mega-doses of the “sunshine” vitamin. “Clinicians still have latitude to make individualized recommendations for higher amounts for their patients, but the public health guidelines are saying that most of the population should not be taking high doses or getting blood screening tests regularly because there is no evidence to support that,” says Dr. Manson.
New evidence on the horizon
Experts are hoping a comprehensive trial underway called VITAL (VITamin D and OmegA-3TriaL) will reveal the true health benefits of vitamin D. Dr. Manson is lead investigator for this large-scale U.S. study among 10,000 adult women over 55 and 10,000 men over 50. She and her colleague, Julie Buring, DSc, are investigating if taking daily doses of 2,000 IU of vitamin D or a supplement of omega-3 fatty acids (Omacor fish oil, 1 gram) can reduce the risk of developing cancer, heart disease and stroke in healthy people with no history of these diseases.
The study is a randomized, double-blind, placebo-controlled trial where the test groups and the comparison groups will have a large enough difference in vitamin D levels to see if there is a meaningful difference in health outcomes. The study began in 2008 and is collecting data over an average of 5 years. The National Cancer Institute and the National Heart, Lung and Blood Institute are primary sponsors for the VITAL Study and final results are expected in late 2017.
Right now, the excitement about vitamin D is focused on the promise it offers in helping with a host of health conditions beyond bone health. “The enthusiasm is definitely outpacing the evidence,” notes Dr. Manson. “Although we know that vitamin D deficiency needs treatment, there is a disconnect between the observational studies that have linked low vitamin D to nearly every known health condition and the randomized trials of high-dose vitamin D supplements that have been largely disappointing to date. We do need the large-scale randomized trials, though, to test rigorously whether supplementation above the recommended dietary allowance confers greater health benefits.”
© Copyright Jane Langille. Originally published on MedShadow.org: May 29, 2014